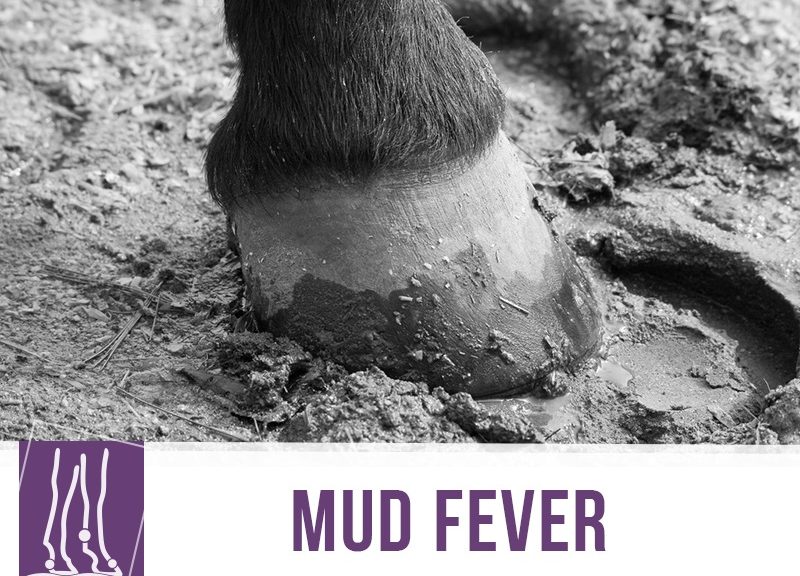
With the colder months fast approaching, it’s always good to remember some things that might affect your horses during this weather.
Mud Fever is actually part of a series of conditions that make up Equine Pastern Dermatitis (EPD) and it can be caused by many different factors.
This condition shows up during spring and winter and to better understand it, we need to know that mud fever isn’t a diagnosis exactly, it’s how the pastern reacts to damage.
That is to say, there is an underlying cause that needs to be investigated when we realise that our horse has signs compatible with mud fever.
EPD can have several forms:
- Mild – Lack of hair in the area, dry scales and crusts. Might also have thicker skin, itchiness and pain (This is what we readily recognise as Mud Fever)
- Exudative – Reddening of skin, lack of hair with the presence of pus or other exudates. (Also called grease heel or dew poisoning)
Owners of draft breeds like Clydesdales or Shires know they might be prone to a third form of Equine Pastern Dermatitis which features the proliferation of excessive tissue in the form of nodular lesions because of issues in the lymphatic system that drains fluids from the limb. This form, more frequent in draft breeds, is commonly called grapes or verrucous pododermatitis and it may progress to the entire lower extremity. The prognosis for this condition is poor because horses often develop secondary infections, it has a poor response to therapy and eventually becomes debilitating for the horse.
There are many root causes of Mud Fever, and Equine Pastern Dermatitis like:
- Genetic and environmental disposition
- Infectious agents, physical or chemical irritants, cancer
This is perpetuated by secondary bacterial and parasite infections, pathologic changes to the skin and a less than ideal environment.
Be on the lookout for these important changes during these seasons. Treatment and positive resolution depend on identifying what is causing Mud Fever and fixing it, so don’t hesitate to contact your vet!
Via: “Mud Season” by RogerGoun, was built upon and is licensed under CC BY 2.0
Would you like to know more about horses? Check our Equine Courses: